Journal entry by Lisa Ryan —
I haven’t written in a while as I was hoping to have a clean update post-surgery but as the weeks have ticked by and folks have asked me my status, I figured it was worthwhile to share what I do know. I have recovered well from my surgery in February. The GREAT news is that the pathology report on the 6.3x3.2x1.2 cm mass that was taken showed a pathological complete response (PCR) to the chemotherapy. This is what we had hoped for as it proves what we could actually see: that the cancer that presented over the summer responded to the chemo.
The pathology also showed still existing lobular carcinoma in-situ (LCIS) and atypical lobular hyperplasia (ALH) but my oncologist said this was not concerning since we already knew the existence of the HER2+ spread and Stage III cancer. I learned that the LCIS does not respond to chemo but it is not a “new” cancer. For that reason, there is no need to add a new chemo at this time but we will continue with the planned treatment of maintaining the herceptin and perjeta infusions every three weeks through the year (concluding September) if my body continues to tolerate it well. My understanding is that this is the best protocol due to the aggressive nature of the HER2+ cancer. I will still need echocardiograms every 6 weeks to watch my heart and will just monitor the diarrhea and digestive issues as these allegedly get progressively worse. (I am still looking to connect with other women who have been through this to find out more.)
What is unclear is the decision regarding radiation. I underwent a lymphoscintigraphy looking for alternative sentinel nodes before surgery (I had a sentinel node biopsy in 2019 with mastectomy so they are looking to see where lymph activity may be redirected). The CT showed radiotracer activity at the intramammary node. However, as this lymph node is located under the sternum, the surgeon stated they would not be able to access that lymph node (“as the chance of morbidity is too high” okay…). But clearly it raises some concerns that it could also be a sign of spread. However, I still have not received an answer as to whether radiation is being recommended.
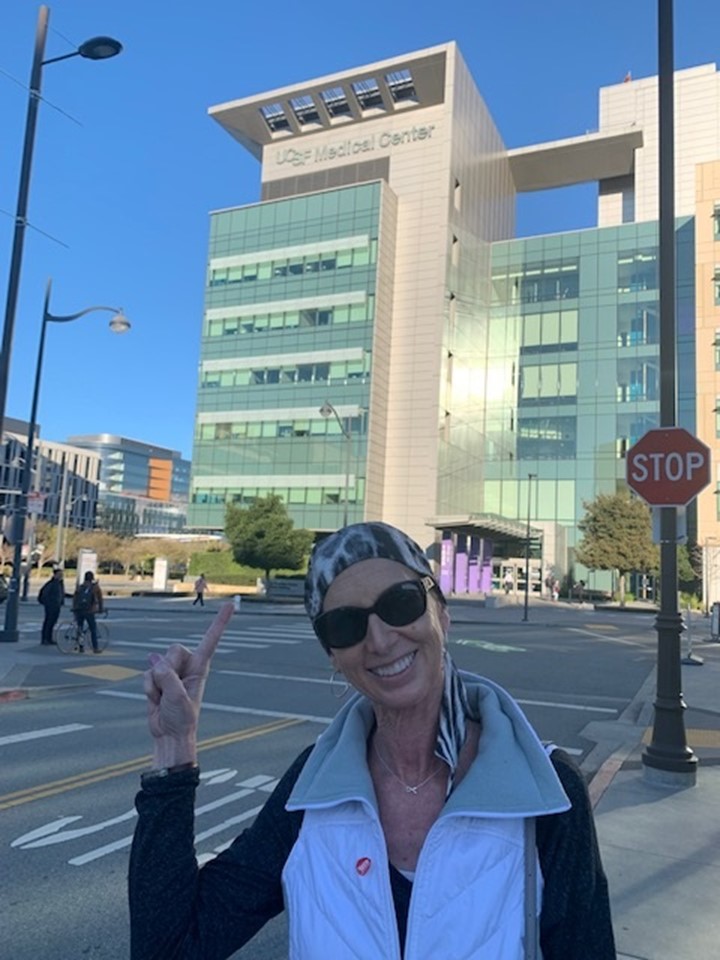
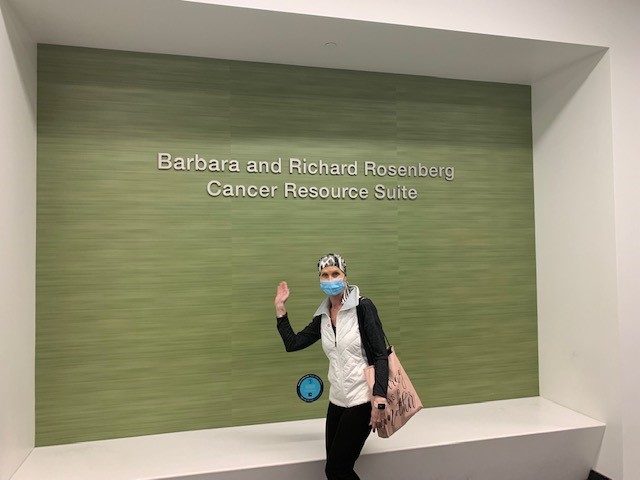
The other good news is that while I will still be under the care of my oncologist at UCSF, I am able to continue my infusion treatments locally. Ironically, my UCSF surgeon recommended an oncologist in Folsom for that treatment, who happened to be my original oncologist in 2019 – small world! So hopefully I bid adieu to UCSF for the time being. While I appreciate the care I received from the wonderful nurses at the oncology infusion center, I will not miss spending literally 4-6 hours in traffic driving to SF every three weeks.
Overall, I am feeling grateful and optimistic. God is good. I also never forget how fortunate I am to be fighting this battle in 2022 and not 2002. I thank the amazing biomedical researchers, scientists, doctors and all involved in developing targeted therapies. While we may not have a complete cure, I know I am blessed to be fighting this fight because of the research and development that has been done over the decades and continues to be done daily!
I haven’t written in a while as I was hoping to have a clean update post-surgery but as the weeks have ticked by and folks have asked me status, I figured it was worthwhile to share what I do know. I have recovered well from my surgery in February. The GREAT news is that the pathology report on the 6.3x3.2x1.2 cm mass that was taken showed a pathological complete response (PCR) to the chemotherapy. This is what we had hoped for as it proves what we could actually see: that the cancer that presented over the summer responded to the chemo.
The pathology also showed lobular carcinoma in-situ (LCIS) and atypical lobular hyperplasia (ALH) but my oncologist said this was not concerning since we already knew the existence of the HER2+ spread and Stage III cancer. I learned that the LCIS does not respond to chemo but it is not a “new” cancer. For that reason, there is no need to add a new chemo at this time but we will continue with the planned treatment of maintaining the herceptin and perjeta infusions every three weeks through the year (concluding September) if my body continues to tolerate it well. I will still need echos every 6 weeks to watch my heart and will just monitor the diarrhea and digestive issues as these allegedly get progressively worse. (I am still looking to connect with other women who have been through this to find out more.)
What is unclear is the decision regarding radiation. I underwent a lymphoscintigraphy looking for alternative sentinel nodes before surgery (I had a sentinel node biopsy in 2019 with mastectomy so they are looking to see where lymph activity may be redirected). The CT showed radiotracer activity at the intramammary node. However, as this lymph node is located under the sternum, the surgeon stated they would not be able to access that lymph node (“as the chance of morbidity is too high” okay…). But clearly it raises some concerns that it could also be a sign of spread. However, I still have not received an answer as to whether radiation is being recommended.
The other good news is that while I will still be under the care of my oncologist at UCSF, I am able to continue my infusion treatments locally. Ironically, my UCSF surgeon recommended an oncologist in Folsom for that treatment, who happened to be my original oncologist in 2019 – small world! So hopefully I bid adieu to UCSF for the time being. While I appreciate the care I received from the wonderful nurses at the oncology infusion center, I will not miss spending literally 4-6 hours in traffic driving to SF every three weeks.
Overall, I am feeling grateful and optimistic. God is good. I also never forget how fortunate I am to be fighting this battle in 2022 and not 2002. I thank the amazing biomedical researchers, scientists, doctors and all involved in developing targeted therapies. While we may not have a complete cure, I know I am blessed to be fighting this fight because of the research and development that has been done over the decades and continues to be done daily!
A $25 donation to CaringBridge powers a site like Lisa's for two weeks. Will you make a gift to help ensure that this site stays online for them and for you?