Journal entry by Kayla Stenstrom —
Gumby Disease
This past week has been a whirlwind of appointments and phone calls. I had two sessions of naturopathic physiotherapy, an appointment with a new pelvic floor physical therapist, a long phone call with an orofacial specialist, and a session with my pain psychologist. I communicated with a compound pharmacy, a naturopath pharmacy and two regular pharmacies, visiting all four of them twice. I also brought both kids to the dentist. Between that, I managed to still work about 35 hours and…I dislocated my left knee. (Squeeze in a visit to orthopedics.)
But what happened at Mayo Clinic?
Familiar with Captain Underpants? I’ll steal a phrase from Dav Pilkey and say, “Now, before I tell you that story, I need to tell you this story.”
It appears that I actually subluxated my knee cap about three weeks ago. That would explain the six-minute episode of sheer pain and inability to bend my knee when I stood up from the couch. Stood up from the couch? Yes. No high impact sports. I just stood up.
Since then, my knee has been throbbing, aching, especially when it’s bent for too long. (When I drove home from Rochester, I had to have the seat back far enough from the wheel to periodically extend my leg.) Well, I got it checked, all good on the x-ray –– can I add that no scan has shown anything useful in the last two years –– but the ortho doc thinks the knee cap slid and got caught on my femur and now the bones are bruised, thus the throb. When he told me that the treatment was physical therapy (and a knee brace), I said, “I’m sorry, but I need to cynically laugh for a moment.” He said, “Have you ever been tested for Ehlers-Danlos syndrome?”
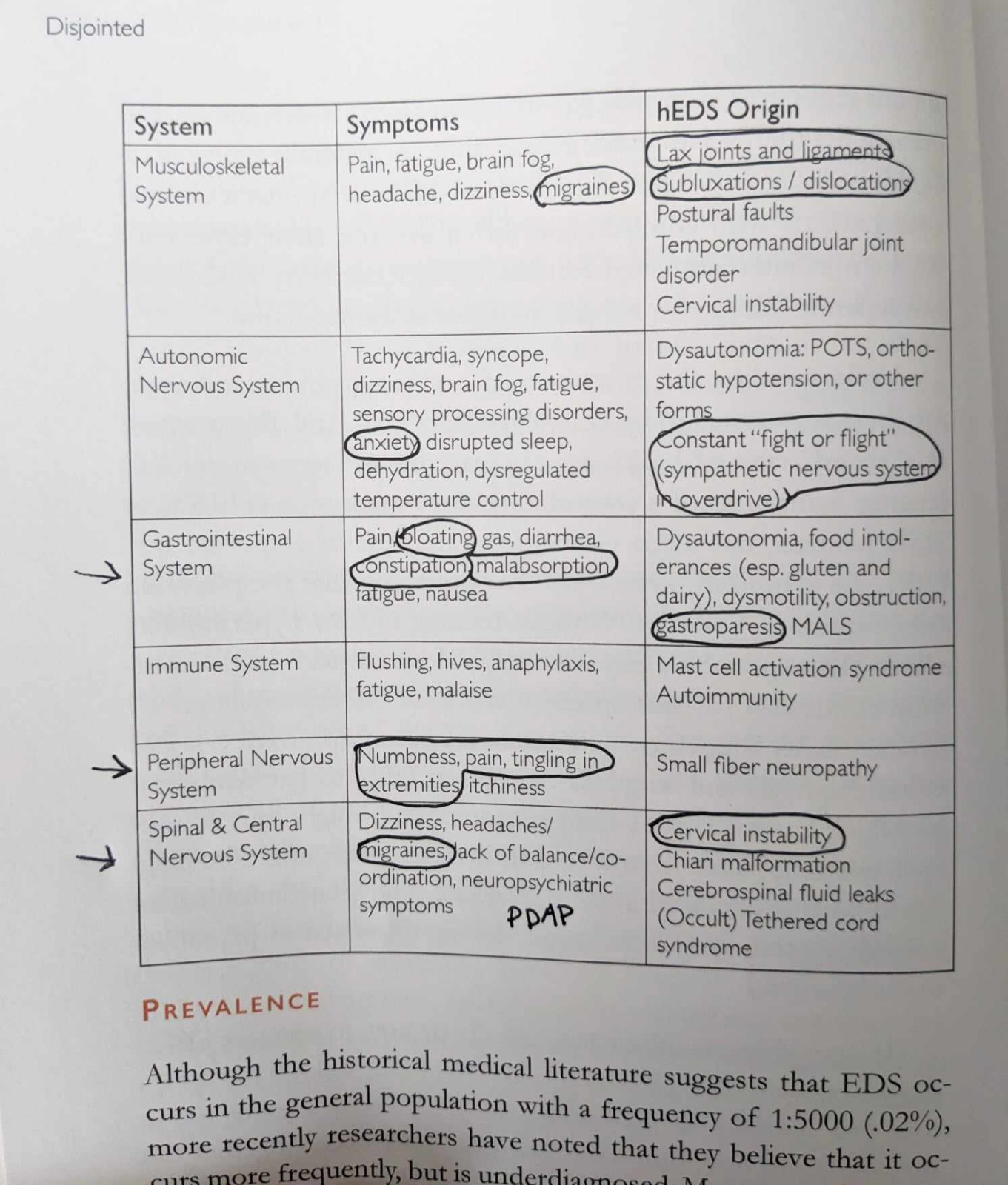
Now, if you’ve followed along for quite some time, you might remember that a quirky hematologist suggested in July 2022 that I have a connective tissue disorder. Well, another big box has been checked for that theory. (If you Google EDS, you’ll mostly see details about skin. There’s much more to it then that. See attached photo of chart) I might literally be falling apart. (I can’t wait to get the sticker of the EDS gang symbol. See attached photo.) (When I told my Dad he said, “I knew you had Gumby disease.”)
How About Some Therapy?
That’s the pre-story.
Now the main story, referencing the satirical laugh above.
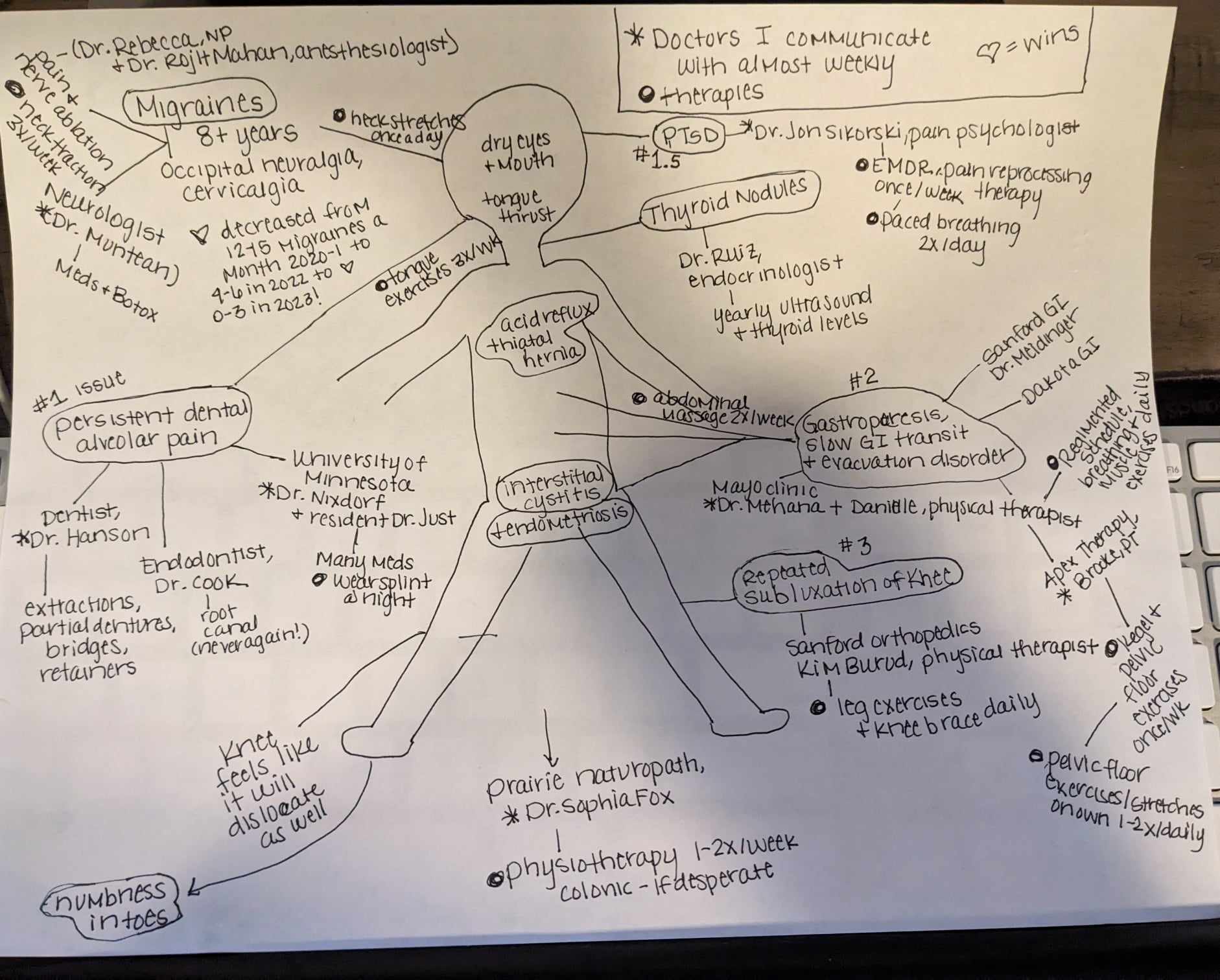
I cackled because here are the “therapies” I already do: neck stretches once a day and neck traction device three times a week for migraines, tongue exercises three times a day and wear a splint at night for tongue thrust, energy healing with Power of 8 group 2-3 times a month, paced breathing two times a day, naturopathic therapy 1-2 times a week, regimented breathing and muscle exercises on the toilet three times a day for evacuation disorder, pelvic floor therapy once a week with exercises at home twice a day for pelvic floor dysfunction, abdominal massage twice a day, walk or exercise daily, pain reprocessing therapy and/or EMDR once a week for trauma. (I lost track so needed to draw a mind map, attached, and a daily schedule of medications and therapies.) I guess I’ll do some leg lifting, too.
Wow. That’s nuts. But how’s your stomach and intestines?
Hang on. Sleep study update: Nothing abnormal found – no upper airway resistance or apnea. I have 94% successful sleep, whatever that means. My interpretation – the doctor voice in my head: "Your body sucks at everything but you're really good at sleeping." (The notes say that my legs don’t move at all when I’m out. I think that’s funny. They’re just bricks for eight hours.)
Mayo Clinic Round Three
Okay, now how was Mayo?
It was good and hard and not helpful and helpful.
I remember when Kevin went to treatment and he said that he wished they would just admit him so he could dive deep and be fixed. I longed for my trip to Mayo to be a dive deep (I did have tubes up my butt most of the week) and the fix that my doctor guaranteed. For months, as I remained eight months pregnant without a baby, he promised, “Physical therapy will resolve this.”
I did learn a lot, about what muscles I should actually be moving and how I should be breathing. I now use that knowledge daily. Like Kevin being launched into the world with awareness of his triggers, I was sent home with knowledge of my breathing and we both set forth with a better connection between our brain and our body.
But I think it’s going to take a long time and a lot more to get better.
While at Mayo, I did demand to see my doctor. I do believe that the PT will make a notable difference, but in the meantime, when I can’t feel anything to practice evacuating, how will we get the liquid, gas and stool that’s continually trapped at my sternum to move its way down? After some negotiating, he agreed to switch me to a new med. Insurance rejected coverage. We appealed. And we won! I took the first pill of Motegrity tonight. (I took Linzess for two months with no improvement.) I am banking a lot on this medication. I can’t keep living on emptying my body with a machine.
Covid is Crap
On the nerve front. This is a complicated update so buckle up.
I had Covid at the end of September. Likely because of it, my nerve pain significantly increased the first week of October and, when not doing PT or pretending to be fine to co-workers and friends, I was largely incapacitated from Oct. 4 to Oct. 21. I could not tell you how I drove to Rochester and back, how I worked, how I functioned. I just did. Because I had to. But I cried a lot and had at least one pain-induced panic attack a day.
The week of Oct. 11, I contacted my team at the University of Minnesota and said I needed to talk to them immediately. The resident assigned to me (I got a new one in Sept., third I’ve had) called me after her patients on Oct. 18. She didn’t know what else I could do beyond taking my current cocktail of Low Dose Naltrexone, Pregabalin, Amitriptyline, and Ketamine. She admitted fear that I was alone in Rochester and sounding suicidal. I assured her that I had no intentions of leaving my children, but that we needed to brainstorm now. She had me call the clinic in the morning to schedule. The appointment was set for Nov. 17.
The Only Guy Who Knows What To Do
On Oct. 23, I emailed her begging her to pull some strings to get me in sooner. On Oct. 25, Dr. Nixdorf, her overseeing physician and the expert on persistent dental alveolar pain (PDAP), called me after work. I was really surprised. He had never contacted me directly before. (I usually meet with the resident and then he comes in for the last 1/3 of the appointment.) I gave an update on the meds I’m on, how I’m doing, etc. and asked “Do you have any other patients on multiple pain meds who are still experiencing the level of pain that I am?” He said, “No. You are my most complex patient.”
That is both validating and terrifying.
I told him I was near ready to pull another tooth and asked him for his reaction, knowing that he’d highly advise against it because we know (from two previous extractions) that the pain just moves to the next tooth to the left and if all lower teeth were removed, I might still feel nerve pain. What’s more, I could lose jaw bone over time and reach a point where the way I look, talk and eat is dramatically different. And, it’s likely that my body wouldn’t tolerate a denture (I’ve chalked up three failed partials, four failed bridges and countless failed retainers). He said, “I can understand that. It’s justified.” I was a bit shocked. It was the first time he had ever said anything other than “That’s really not advised.” in response to talk of extracting. He followed it with “I have some patients who pull another tooth, the pain is gone and they wish they had done it a long time ago. I have other patients who pull a tooth and the pain continues or gets worse. I don’t know which you would be.”
He also said, “If you want to get a second opinion on all this, it’s okay.” I told him that no dental specialist in Fargo-Moorhead has heard of PDAP (0.03% of people have it) and the colleagues that my sister has met at national dental conferences all say to go to Nixdorf.
Dr. Nixdorf explained how his team approaches PDAP:
- Anticonvulsants / nerve medication (Gabapentin or Pregabalin)
- Anticholinergic medication (like Amitriptyline)
- Botox in the mouth
- Psychiatry (all his PDAP patients have a history of depression and anxiety)
- Topical numbing agents
- Ketamine (newest and very much in experimental phase)
I have tried all of the above. (EDS can involve malabsorption so I do wonder if the reason that max doses of so many medications don’t work for me is because of a larger issue.) We talked through each, what we could change, what we could not, and landed on this plan:
- Pregabalin keeps me alive. Stay on max dose.
- Wean off of Amitryptline due to adverse effects and its notoriety for causing constipation. Add back med for depression and anxiety.
- Fight insurance for approval to have U of M administer Botox on the tongue-side of my lower teeth.
- My neurologist administered Botox on the lip side in June, using what was left of the solution after he injected into the spots dictated by migraine protocol, and telling insurance that the mouth injections were for migraines. Shh.
- What he had left to inject in my mouth was probably not enough or in the right spot to make a difference.
- My neurologist administered Botox on the lip side in June, using what was left of the solution after he injected into the spots dictated by migraine protocol, and telling insurance that the mouth injections were for migraines. Shh.
- Increase frequency of sessions with pain psych.
- Try another topical compound.
- Increase Ketamine very slowly so that I can take it during the day without getting high.
- Should be an interesting experiment
So here we go, with all the plans and all the steps. And here is my family, trying to be strong.
Our Family
I’ll be even open book as usual: our family is hurting. For two years, Kevin and the kids were adaptable and patient and resilient. They are crumbling. The kids fight with each other and we with them a lot. Cali is exhibiting worrisome signs of increased depression: apathy, disinterest in all activities, not hungry, mood swings, crying multiple times a day. Ian sobbed in my arms tonight, saying “I just want to be with you Mom.” Kevin is trying to react to the kids' increased behaviors then feeling guilt and despair, like he's mostly angry in interactions with them. (Additional layer: The week before I went back to Mayo, Kevin worked 65 hours, being on call 24/7 for beet harvest.) We all feel alone even though we are geographically in the same house. I think that there is only so long that a family can watch one of its members suffer, and experience the life disruption of it.
One of the major limitations to improvement of this situation is just time for appointments. As I look at my calendar, I see that I have had 1-4 doctor appointments each week for the last 25 months! I currently see 11 doctors regularly and saw 22 different doctors in the last two years. (I did a little math and I think that’s at least 540 hours of appointments! It’s probably 5.2 million forms that I’ve filled out.) This does not count any physical therapy, counseling, dental, orthodontic or optometry appointments that I took the kids to. I have had to postpone myofunctional therapy that Ian needs and more counseling for Cali because I don’t have time to bring them there. This kills me.
Kevin and I feel far from being the parents we long to be. We have things we wish to accomplish professionally. Not getting to be how we want to as parents and within our careers is a process of grieving the loss of ourselves.
You Made It to the End!
Some of my desires are simpler. I want to sing in church rather than staying silent to bank the chances I have to talk. I want to talk over dinner with friends without my mouth hurting and I want to talk as much as I want to my kids without paying for it the next day. I want to take less than 18 pills a day. I want my clothes to fit. I want to poop.
I know this story is heavy. I know it sounds incredibly pessimistic. I know it sounds like we don’t have hope.
It is heavy. It is what it is and I aim to be frank. We do have hope. We focus on taking the next step with the information we have and the best attitude we can muster, knowing you are with us.
We cannot thank you enough for your words, your gifts, your time, your energy and your love. I receive personal messages every day and it means a lot. I also deeply value the connections I've been able to make with others in chronic pain or illness – thank you for reaching out to me with your stories. Let's keep sharing ideas and hugs.
-
Keeping track of doctors and therapiesPatients and caregivers love hearing from you; add a comment to show your support.Help Kayla Stay Connected to Family and Friends
A $25 donation to CaringBridge powers a site like Kayla 's for two weeks. Will you make a gift to help ensure that this site stays online for them and for you?
Show Your Support
See the Ways to Help page to get even more involved.