Journal entry by Evonne Edwards —
2023 was one of the hardest years of my life --- certainly the most challenging physically. I'm thankful to get to see 2024, grateful for the treatments, physicians, family, and friends that have made that possible.
I wrapped up my (hopefully!) last chemotherapy treatment at the end of September. By that point, my body was ravaged by the effects of chemo and my blood counts no longer reaching normal between treatments. My energy levels had dipped so low that my oncologist ordered an echocardiogram before my last treatment to check on my heart functioning. Thankfully, my heart function remained within normal limits despite being decreased by the effects of chemo (one of the most effective chemo meds is known to cause heart damage) and I was able to complete my last round. I continued to get intense headaches from the last of my chemo meds, so my oncologist also ordered an MRI to ensure we were not missing anything in my brain --- thankfully, that too was clear.
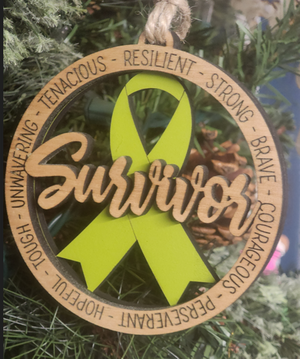
At the end of October, I had a posttreatment PET scan. Not only was it clear, but my Deauville score was 1. Deauville scores measure the update of radioactively-labeled glucose, are used to assess treatment response, and range from 1 (no/minimal uptake) to 5 (markedly increased uptake); generally, 4-5 = cancer, 3 = ambiguous, 1-2 = not cancer/no more metabolic activity than most tissue. I was at a 2 on my mid-treatment PET, so getting down to a 1 was great! At my October appointment, my bloodwork was also looking good. I was officially declared to be fully in remission! While there are no guarantees and my chance of recurrence may be as high as 10-20%, my oncologist was pretty confident/hopeful that I will remain in remission and approved me to get my chemo port removed (scheduled for early February).
The last two months has been a slow recovery. Chemo is a gift that keeps on giving and some days the litany of annoying and frustrating aftereffects can be discouraging. The most limiting and persistent symptom is low energy -- though slowly improving, I'm still quickly exhausted by even minimally physical tasks, like folding clothes and even moderate walks. Yet chemo is a gift --- one that has absolutely saved my life.
I have returned to work part time and have slowly worked my way up to 25-30 hours/week. I'm hoping to be able to begin working my new "full-time" at 32-36 hours in the next couple of months. I am incredibly thankful for a job that I can generally do from home on low energy days and take breaks when my energy lags. My managers/supervisors have been amazingly supportive throughout this journey, and we continue to figure out what I'm able to do. I have not yet resumed seeing patients, but I hope to be able to do so early in the new year. My mom has begun going home to Iowa for longer stretches -- up to 2-3 weeks at a time --but continues to help with the girls and assist Mark and me in preventing absolute chaos in our home when she is here.
My delay in this update is reflective of my energy state -- between work and parenting and finding ways to take care of my health in this new normal, I often have little energy remaining.
Instead of a year in review (which would be relatively short beyond my battle with cancer!), here is part of my gratitude list:
- Being able to enjoy my daughter's birthdays before/at the beginning of this journey
- A vacation a mere couple of weeks before the lymphoma pain began -- the trip to Virginia to see the historic triangle (Jamestown, Colonial Williamsburg, and Yorktown), go to Busch Gardens, and visit Mt. Vernon with the girls and my mom was full of wonderful memories to hold on to in the darkest times
- A year of sacrificial care and support from my mom (and the loving support of my stepdad that supported this!)
- The steady love of my husband
- The best in-laws I could imagine -- supportive visits from my sisters-in-law and their families, care packages and endless support and wisdom from the lived experience of my mother-in-law, and the decades of clinical knowledge from my hematology-oncologist father-in-law
- Pine Rest -- including the support of HR, benefits that helped keep us afloat in the months and months when I was unable to work, a CEO and CMO who called to check on me and help me how they could, wonderfully supportive managers/supervisors, and coworkers and current/former psychiatry residents who blessed me with brimming gift baskets, care packages, and meals.
- A community that gives generously and has a fund to help with cancer medical bills
- Gilda's Club and the community it supports -- especially at the beginning and summer camp for our girls
- Amazing family and friends who showered me with support, gave generously to my GoFundMe account, took my girls to school on early treatment days, checked in on me, sat with me on chemo days, encouraged and prayed for me as my hair fell out and body got ground down, and helped me and my family in ways I am still trying to wrap my head around
- Timing of cancer that allowed me to avoid colds and flu season during active treatment and be able to spend needed time with family at Christmas
- Lemmen Holton Cancer Pavillion -- the wise doctors and caring nurses who still walk with me, the palliative care team that ameliorated the endless symptoms from cancer and chemo, the oncology psychologist who guided me through the emotional turmoil of this year, and the myriad of perks and services provided
- The many prayers of so many people
- Our loving God and His consolation, healing, peace, comfort, and faithfulness
In a time that remains full of uncertainty, New Year's resolutions seem a bit foolhardy. Instead, here are my New Year's hopes: That remission will be sustained, my healing complete and 2024 will be a year not only free of illness/cancer but a year of health, balance, and recovery.
A $25 donation to CaringBridge powers a site like Evonne's for two weeks. Will you make a gift to help ensure that this site stays online for them and for you?