Journal entry by Jon and Megan Nelson —
E L E N A * U P D A T E
It’s been a while since I have shared an update on Elena’s health status. We had a recent virtual appointment with her pulmonologist (lung doctor). I am very happy and even more thankful to report that she is doing great. We have all been home since March meaning she has not been exposed to all the germs that come with daycare life. We are very happy about this as it is just so much less stress than last winter. When we were discharged from Mayo we were told that for her first four years of life it was crucial that we take extra care to protect her from exposure to respiratory illness to the best of our abilities (challenge accepted 😉).
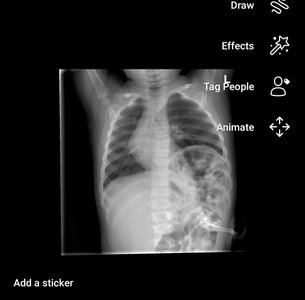
Ok, where am I? Oh yeah, her appointment last week. We have had ongoing concerns related to the abnormal structure of her chest wall/rib cage and it was time that we had them addressed. Elena’s left chest (hernia side where she now has a paralyzed diaphragm due to the large hole that was repaired) appears sunken in compared to the right side that appears pushed out. Along with this she has some rib flaring and indentations, enough to make any parent go a bit crazy with worry. The doctor was really great at reassuring our concerns. She explained that obviously the right side of her chest is protruding because in utero all of her organs were pushing up and shifting everything to the right and because her repaired diaphragm is paralyzed there continues to be more pressure up into the chest cavity than there would be for a typical person. She reassured us that this is ok as it is not causing Elena any trouble…. whew. She also explained that another reason why the left side is more sunken is because of the difference in her intercostal spaces (area in between ribs) on that side. The spaces are smaller with less muscle mass due to her having a substantially smaller lung on the left as well as a paralyzed diaphragm. Those muscles just aren’t being contracted as much and are smaller as a result.
The conversation soon turned into a more positive one (thank goodness) as we discussed how all of this may impact her spine. It is not unheard for CDH babies to develop scoliosis later in life for a variety of reasons that I won’t go into. The doctor pulled up her most recent X-ray and said “See, look at that, her spine is as straight as an arrow.” This statement had me in tears (happy tears) because with everything that she has faced Elena has exceeded our expectations and though I worry (as any parent would) I am often reminded that God has been with us every step of the way, continues to be with us and has great plans for Elena.
I often think of the Bible verses in Psalm 139: 13-16 “13 For you created my inmost being; you knit me together in my mother’s womb. 14 I praise you because I am fearfully and wonderfully made; your works are wonderful; I know that full well. 15 My frame was not hidden from you when I was made in the secret place, when I was woven together in the depths of the earth. 16 Your eyes saw my unformed body; all the days ordained for me were written in your book before one of them came to be.”
Elena continues to have her G-tube but has recently weaned from needing it for calories. We started a weaning plan with an independent group called “Growing Independent Eaters” in early November as we weren’t gaining much ground using the conventional route and just really didn’t see an end in sight with that. After starting the wean we only used the tube for milk/calories about 10 times and a bit than that for fluid/water support. About mid-December when she was declared officially weaned. She still has it in place as she needs to show that she can gain weight and sustain that for a period of time before it would ever be removed. I have no doubt she will continue to do great with that. Thank you all for your continued prayers.
Photos show her before her repair surgery, immediately after and then as time has passed and the repair has weakened some.
A $25 donation to CaringBridge powers a site like Megan and Jon's for two weeks. Will you make a gift to help ensure that this site stays online for them and for you?